Get Healthy!
Staying informed is also a great way to stay healthy. Keep up-to-date with all the latest health news here.
17 Sep
Marijuana Use May Spike Type 2 Diabetes Risk
A new study finds pot users are nearly 4 times more likely to develop type 2 diabetes compared to the general public.
16 Sep
Could Ditching Daylight Saving Time Improve America’s Health?
Researchers compare three hotly debated time policies and find a surprising winner when it comes to improving health outcomes for millions of people.
15 Sep
GLP-1 Medications in Kids: Promising Health Results, Ongoing Safety Concerns
A new study finds children and teens with obesity or diabetes who take GLP-1 weight-loss medications experience significant improvements in many cardiometabolic risk factors, but long-term safety questions remain.
Hair Samples May Help Spot Mental Health Risks in Sick Kids
Children with chronic illnesses face extra challenges, and measuring stress through hair samples may help doctors predict which kids are at highest risk for mental health problems.
Researchers studied 244 Canadian children with chronic physical illnesses such as diabetes, arthritis and cystic fibrosis. Over four years, the team measured co...
- I. Edwards HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
FDA Cracks Down on Hims, Other Telehealth Companies Over Drug Ads
Federal health officials are cracking down on telehealth companies’ promotion of unapproved versions of prescription drugs, including popular weight loss medications.
On Tuesday, the U.S. Food and Drug Administration (FDA) released more than 100 warning letters aimed at both drugmakers and online health companies. Among them: Hims &a...
- I. Edwards HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
DermaRite Widens Recall to 32 Products Over Bacteria Risk
DermaRite Industries has widened its earlier recall of hand soaps to include 32 personal care products that could be contaminated with a dangerous bacteria, health officials report.
The New Jersey-based company said the recalled items include body washes, lotions, soaps, shampoos, sanitizers and wound cleansers sold nationwide and in Puert...
- I. Edwards HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
Wegovy May Help Quiet Constant Food Cravings, Study Finds
A popular weight-loss drug may do more than help patients shed pounds. It could also help quiet the nonstop food cravings many people struggle with.
New results from a U.S. survey of 550 Wegovy users found that patients reported a major drop in “food noise,” or intrusive thoughts about food, after starting the drug.
- I. Edwards HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
Pregnant Women With Epilepsy Not Consulting With Neurologists, Missing Out On Important Care
Roughly half of pregnant women with epilepsy see a neurologist while they’re expecting, an oversight that could put both mom and baby at risk, researchers say.
About 45% of women with epilepsy didn’t see a neurologist at all in the year leading up to delivery, researchers reported this week at a meeting of the American Neurolog...
- Dennis Thompson HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
Sleep Difficult For LGBTQ+ Teens, Study Says
LGBTQ+ teenagers in the United States might be losing sleep due to violence, bullying and rejection, a recent study says.
Gender and sexual minority teens are more likely to have trouble falling asleep at night, researchers reported in June in the Journal of Adolescence.
However, those teens who experienced more warmth and s...
- Dennis Thompson HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
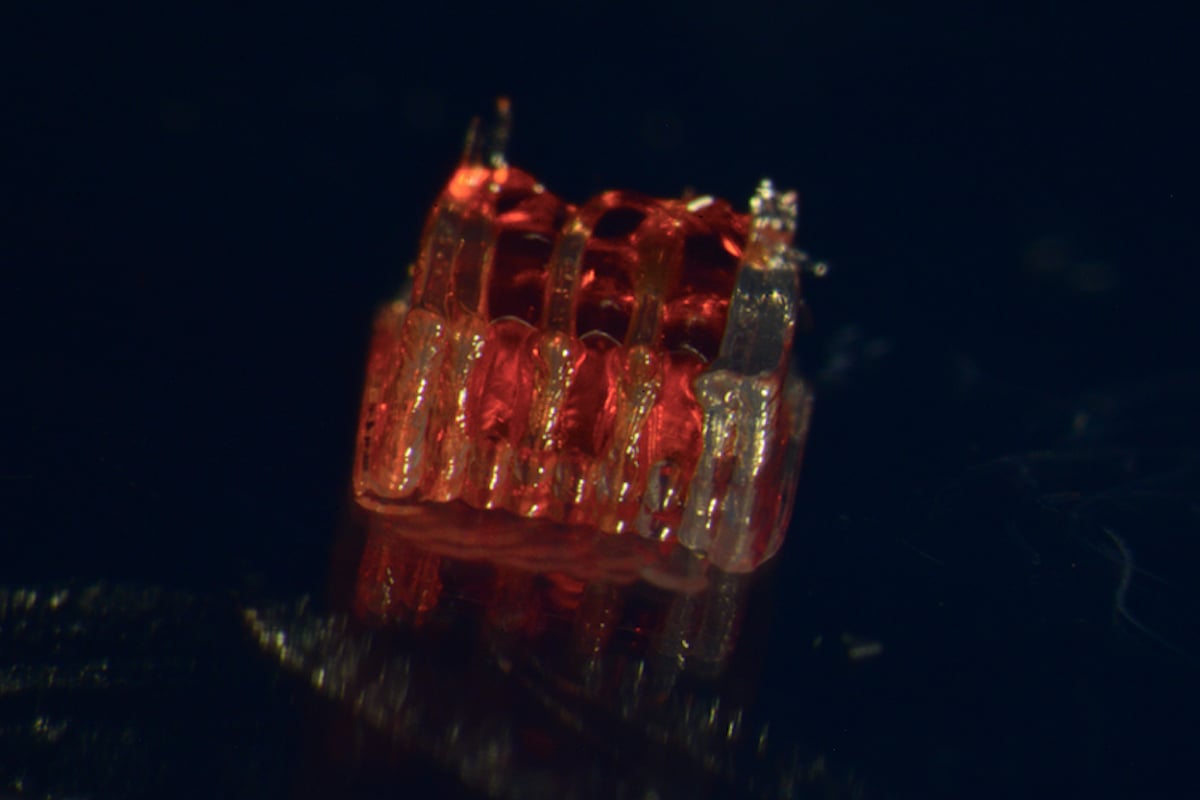
3D Printing Offering Hope For Spinal Cord Injuries
A new process that combines 3D printing, stem cells and lab-grown tissues could prove a groundbreaking innovation for spinal cord injury recovery, a new study says.
The process uses 3D printing to form stem cells into scaffolds containing microscopic channels that guide the growth of new nerve cells along the site of the spinal cord injury...
- Dennis Thompson HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
Can Mammograms Assess Women's Heart Health?
Regular mammograms might offer a “two-for-one” opportunity to protect women’s health, a new study says.
Mammograms can be used to successfully predict heart disease risk in women, on top of their ability to detect early breast cancers, researchers reported Sept. 16 in the journal Heart.
A new AI model using...
- Dennis Thompson HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
Timing Of Menopause Hormone Therapy Key To Protecting Brain From Alzheimer's
Hormone replacement therapy might protect a woman’s brain against Alzheimer’s disease, but only if the timing’s right, researchers say.
Women who start hormone therapy within five years of menopause can lower their Alzheimer’s risk by as much as 32%, researchers reported this week at the annual meeting of the Americ...
- Dennis Thompson HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
Circumcision Down In U.S., Partly Due To Parental Mistrust Of Doctors, Study Says
Circumcision rates have declined significantly in the United States, driven in part by parents’ distrust of medical advice, a new study says.
Circumcision of newborn boys declined from 54% to 49% between 2012 and 2022, according to records from more than 1.5 million U.S. male births.
The trend flies in the face of doctors&rsquo...
- Dennis Thompson HealthDay Reporter
- |
- September 17, 2025
- |
- Full Page
U.S. Officials To Review COVID Vaccine Safety in Pregnancy, Kids
Federal health officials are reviewing safety data on COVID vaccines in pregnant women and children, and may also reconsider recommendations for older adults.
The U.S. Food and Drug Administration (FDA) is analyzing reports of possible birth defects after vaccination during pregnancy, while also preparing a presentation on deaths in childr...
- I. Edwards HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Goodles Mac & Cheese Recalled Due to Hidden Allergen Risk
Gooder Foods, Inc. is recalling eight lots of its boxed mac and cheese products because they may contain undeclared allergens, federal officials said.
The recall covers five lots of Vegan Is Believin’ – Plant Based White Cheddar with Spirals that may contain milk and three lots of the Here Comes Truffle – Creamy Truffle F...
- I. Edwards HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
RFK Jr. Adds 5 Members to Vaccine Advisory Committee Ahead of Meeting
Five new members have been appointed to the U.S. Centers for Disease Control and Prevention’s (CDC) vaccine advisory committee, federal health officials announced.
The move comes just days before the Advisory Committee on Immunization Practices (ACIP) meets to review vaccines for COVID-19 and several other diseases.
The new mem...
- I. Edwards HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Over 100,000 Paris Hilton Mini Fridges Recalled for Fire Risk
More than 100,000 Paris Hilton-branded mini fridges are being recalled because of a risk of fire and burns, federal safety officials announced.
The U.S. Consumer Product Safety Commission (CPSC) said the recall consists of two models of the Paris Hilton Mini Beauty Fridge: A 4-liter version sold in pink, white, aqua and hot pink, and a 10-...
- I. Edwards HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Over-The-Counter Sales Of OD-Reversal Drug Have Been A Bust
Over-the-counter sales have tanked for the overdose reversal drug naloxone, likely due to its high price, a new study says.
Naloxone (Narcan) is a nasal spray that rapidly reverses an overdose by blocking opioid receptors in the body. It has been a key weapon in fighting America’s opioid drug crisis.
To that end, regulators in ...
- Dennis Thompson HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Early Breast Cancer Survivors Have Little Added Risk Of A Second Cancer, Study Says
Women who survive an early breast cancer can breathe easy, a recent study says.
Their risk of developing a second cancer is low, about 2% to 3% greater than that of women in the general population, researchers reported in The BMJ.
“Many breast cancer survivors believe their risks of a second cancer are much higher than...
- Dennis Thompson HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Can Weed Increase Risk Of Type 2 Diabetes?
Weed might nearly quadruple a person’s risk of developing type 2 diabetes, a new study says.
People who use cannabis have a 3.7 times greater risk of type 2 diabetes compared to the general population, researchers reported Monday at a meeting of the European Association for the Study of Diabetes in Vienna.
“As cannabis be...
- Dennis Thompson HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Triple Dose Of Ozempic Safe, More Effective For Weight Loss
A triple-sized weekly dose of Ozempic works better to help people with obesity shed excess pounds without significant side effects, new clinical trial results show.
Obese folks lost more weight taking 7.2 mg of semaglutide (Ozempic/Wegovy) a week than those taking either the currently approved dose of 2.4 mg or a placebo, researchers repor...
- Dennis Thompson HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Researchers: Too Soon To Tell If 'Liquid Biopsies' Help More Than Harm In Cancer Screening
“Liquid biopsy” tests using blood samples to screen for multiple types of cancer are attracting much attention, for their potential to catch unseen tumors.
But it's too soon to tell whether they're truly useful in the fight against cancer, a new evidence review warns.
These multicancer early detection (MCD) tests are comm...
- Dennis Thompson HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page
Permanent Standard Time Could Cut Strokes, Obesity Among Americans
Most Americans would be healthier if the nation dropped daylight saving time, a major new study says.
Switching to permanent standard time would prevent about 300,000 cases of stroke per year and result in 2.6 million fewer people with obesity, researchers estimate in the Proceedings of the National Academy of Sciences.
Perm...
- Dennis Thompson HealthDay Reporter
- |
- September 16, 2025
- |
- Full Page















.jpg?w=1920&h=1080&mode=crop&crop=focalpoint)


