Get Healthy!
Staying informed is also a great way to stay healthy. Keep up-to-date with all the latest health news here.
02 Jul
Top 3 Medical Emergencies At School
A new study identifies three medical emergencies that account for the most EMS calls at schools. Researchers recommend improved training for these target areas.
01 Jul
Childhood Obesity in the U.S. Continues to Rise
A new study finds obesity in kids 2 to 19 years of age increased significantly between 2011 and 2023, and the COVID-19 pandemic was not a main driver.
30 Jun
Regular Exercise Helps Ease Kids’ Depression and Anxiety
A new study finds exercise decreases symptoms of depression and anxiety in children and teens – and may offer an alternative to antidepressants.
Could Dairy Be Causing Your Bad Dreams?
Having bad dreams after eating ice cream or cheese? Your stomach may be trying to tell you something.
New research shows that people with worse symptoms of lactose intolerance tended to report more frequent nightmares, NBC News reported.
The research, published July 1 in Frontiers in Psychology, looked at the eating...
- I. Edwards HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Most Dads Take Two Weeks or Less of Parental Leave, Study Finds
Taking time off work when a baby is born is good for dads and babies alike. But a new study finds that most fathers still don’t take much parental leave — often because they simply can’t afford to.
Just 36% of new dads said they took more than two weeks of leave after their child’s birth, while 64% said they took tw...
- I. Edwards HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Judge Blocks Layoffs at U.S. Health Department
A federal judge has stopped the Trump administration from implementing more layoffs at the U.S. Department of Health and Human Services (HHS), saying the job cuts likely went against the law.
The decision came Tuesday from U.S. District Judge Melissa DuBose in response to a lawsuit filed by attorneys general from 19 states and the District...
- I. Edwards HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Tattoos Don't Convey Accurate Impressions Of People, Study Says
Tattoos have become a form of self-expression, a means of telling the world something about yourself.
Unfortunately, observers mostly misread these inky cues and misjudge the personalities of tattoo bearers, a new study says.
Study participants tended to agree among themselves on what they think a tattoo says about someone, but their...
- Dennis Thompson HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Sleep Apnea Puts Soldiers In Harm's Way
Sleep apnea could be increasing the risks borne by U.S. soldiers serving on the front lines of combat, a new study says.
Front-line soldiers are far more likely to suffer PTSD, anxiety, depression and injuries if they have sleep apnea, researchers reported recently in the journal Chest.
“This study underscores the grow...
- Dennis Thompson HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Livestock Manure Could Be Source Of Antibiotic Resistance, Researchers Warn
Antibiotic resistance is an urgent global public health threat, as more microbes gain the ability to thwart essential bacteria-killing drugs.
And there's a hidden means by which antibiotic resistance is likely increasing, researchers say.
Manure from livestock is a major reservoir for antibiotic resistance genes that could threaten h...
- Dennis Thompson HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
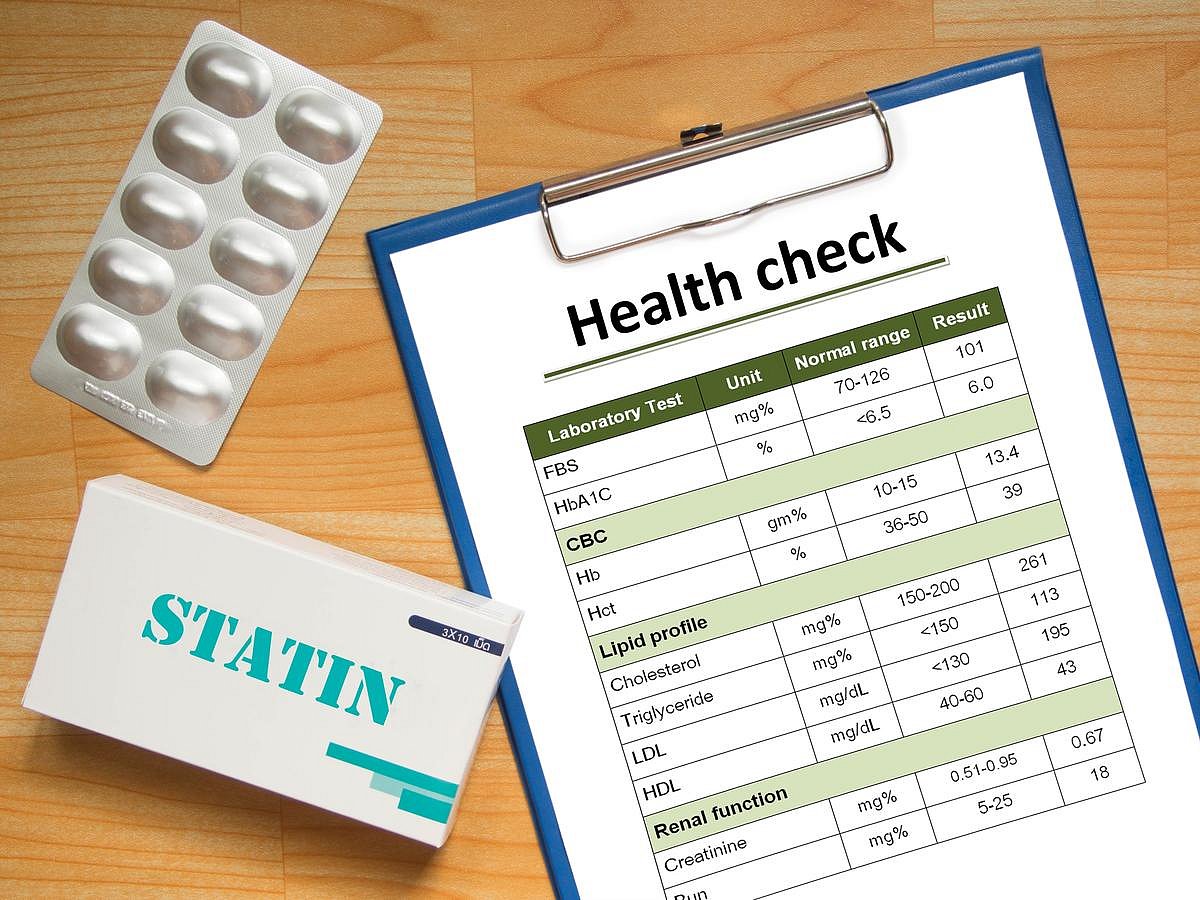
Tens Of Thousands of Heart Attacks, Strokes Could Be Prevented With This Prescription
Tens of thousands of people suffer needless heart attacks and strokes every year because they aren’t taking cholesterol-lowering drugs, a new study says.
More than 39,000 deaths, nearly 100,000 non-fatal heart attacks and up to 65,000 strokes in the U.S. could be prevented if people eligible for statins and other cholesterol-lowering...
- Dennis Thompson HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Brainstorming? Avoid The Internet, Study Says
Want to think outside the box?
Avoid the internet, a new study says.
Googling for new ideas can inhibit a group’s creativity during brainstorming sessions, researchers reported June 30 in the journal Memory & Cognition.
Internet searches appeared to stymie the production of clever ideas in groups asked to bra...
- Dennis Thompson HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Anger Management Improves With Age In Women, Study Says
Remember your sweet-hearted grandmother, who never seemed out of sorts no matter what nonsense landed in her lap?
That’s a skill, and it improves during a person’s lifespan, a new study says.
Women get better at managing their anger as they age, starting in middle-age, researchers reported today in the journal Menopau...
- Dennis Thompson HealthDay Reporter
- |
- July 2, 2025
- |
- Full Page
Trump Administration May Cut Funds to Hospitals Offering Gender Care to Kids
The Trump administration may cut off federal funding to hospitals that provide gender-related treatments to children and teens.
Nine major children’s hospitals recently received letters from federal officials seeking information about procedures such as hormone therapy, puberty blockers and sex-reassignment surgeries, The Wall St...
- I. Edwards HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
Supreme Court Won’t Hear Anti-Vaccine Group’s Free Speech Case
On Monday, the U.S. Supreme Court said it will not hear a case brought by a group once led by U.S. Health Secretary Robert F. Kennedy Jr. that claimed Facebook censored its vaccine-related content.
The Children’s Health Defense sued Meta Platforms, the parent company of Facebook and Instagram. It claimed the company removed their con...
- I. Edwards HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
Moderna’s New Flu Shot Shows Strong Results in Older Adults
Moderna’s new flu vaccine, based on the same mRNA technology used in its COVID-19 shot, showed promising results in a major trial, the company announced Monday.
The vaccine, called mRNA-1010, was tested in a Phase 3 study in adults aged 50 and older. It worked better than a standard-dose flu vaccine, providing 26.6% more protection a...
- I. Edwards HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
AI Can Help Determine A Person's Specific Form Of Dementia
A new AI tool can help doctors hone in on a patient’s particular type of dementia, including Alzheimer’s disease, a new study says.
The AI tool, StateViewer, helped researchers identify a person’s dementia type in 88% of cases, according to results newly published in the journal Neurology.
The tool could he...
- Dennis Thompson HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
Medicaid, Medicare Don't Adequately Cover Addiction Treatment, Study Says
Opioid addicts covered by Medicare and Medicaid are less likely to receive the mental health and substance use treatment that they need, a new study says.
Addicts with public insurance receive more than twice as many sessions if their therapy is also covered by other sources, such as court-mandated treatment, researchers report in the jour...
- Dennis Thompson HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
IBS Rates Nearly Doubled During the Pandemic
The COVID-19 pandemic took a toll on Americans’ guts, researchers report.
Gut disorders like irritable bowel syndrome (IBS) increased significantly during the COVID-19 pandemic, a new study says.
Rates of IBS nearly doubled among U.S. adults, rising from around 6% in May 2020 to about 11% in May 2022, results show.
Other ...
- Dennis Thompson HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
Grip Provides Insight Into Psychosis, Study Says
“Get a grip” might be a truer saying for holding onto sanity than previously thought, a new study says.
A loss of grip strength might be an early sign of psychosis, researchers report in the American Journal of Psychiatry.
People recently diagnosed with psychosis have weaker grip strength compared to folks in goo...
- Dennis Thompson HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
Wildfire Smoke Alters Immune System, Study Says
TUESDAY, July 1, 2025 (HealthDay News) —Exposure to wildfire smoke might make some people more likely to fall ill by altering their immune systems, a new study says.
Fire smoke appears to affect the immune system on a cellular level, researchers report in the journal Nature Medicine.
People exposed to smoke showed an i...
- Dennis Thompson HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
Food Safety is Key for Fourth of July Cookouts
Cookouts on the Fourth of July aren’t just a tradition – they’re expected as part of a day of outdoor games, fireworks and fun.
But a good cookout can turn bad if the potato salad or hamburgers carry a foodborne pathogen that makes friends and family sick, experts warn.
“Summer food safety is often overlooked,...
- Dennis Thompson HealthDay Reporter
- |
- July 1, 2025
- |
- Full Page
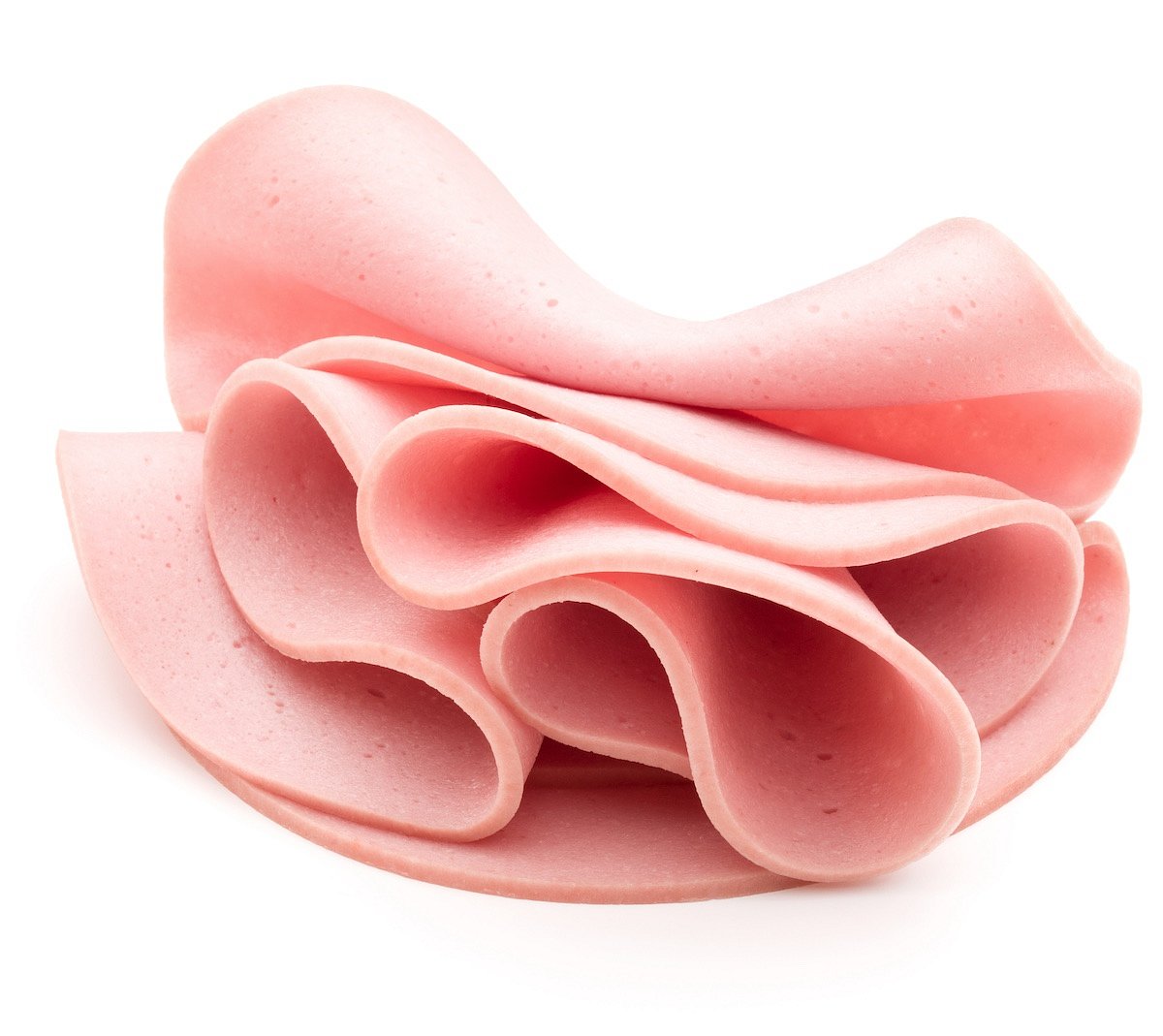
Close to 150,000 Pounds of Ready-to-eat Bologna Recalled Due to Mislabeling
Gaiser's European Style Provisions Inc. is recalling almost 150,000 pounds of ready-to-eat bologna due to mislabeling.
The recalled lunch meats contain meat or poultry source materials that are not listed on the product labels, CBS News reports.
The bologna was sold under various names and labels and was prod...
- Denise Mann HealthDay Reporter
- |
- June 30, 2025
- |
- Full Page
Nestle, Other Food Companies Vow to Ban Artificial Colors
Nestle has joined a growing list of major food companies pledging to voluntarily eliminate artificial colors from their U.S. products by the middle of next year amid mounting health concerns.
"We are always looking for different ways to offer great tasting, compelling choices for our consumers," Nestle's U.S. CEO Marty Thompson said in a s...
- Denise Mann HealthDay Reporter
- |
- June 30, 2025
- |
- Full Page