Get Healthy!
Staying informed is also a great way to stay healthy. Keep up-to-date with all the latest health news here.
08 Jul
How Does BMI Affect Breast Cancer Risk in Postmenopausal Women?
A new study finds the combination of excess weight and heart disease in postmenopausal women is associated with an especially high risk of developing breast cancer.
07 Jul
Untreated High Cholesterol Causing Needless Heart Attacks and Stroke
In a new study, researchers estimate nearly 100,000 non-fatal heart attacks and up to 65,000 strokes could be avoided if people eligible for statins and other cholesterol-lowering drugs were taking them.
05 Jul
Teenage Drivers Spend About 21% of Each Road Trip on the Phone
Researchers surveyed more than 1,100 teenage drivers and found cell phones are a big distraction behind the wheel – even though many are aware of the danger to themselves and others.
Fruits And Veggies Protective Against IBD, Study Says
A healthy plant-based diet might protect people from inflammatory bowel diseases, a new study says.
People noshing healthy plant-based foods had a 14% lower risk of Crohn’s disease and an 8% lower risk of ulcerative colitis, researchers found.
On the other hand, an unhealthy diet containing more animal fats and vegetable oils w...
- Dennis Thompson HealthDay Reporter
- |
- July 9, 2025
- |
- Full Page
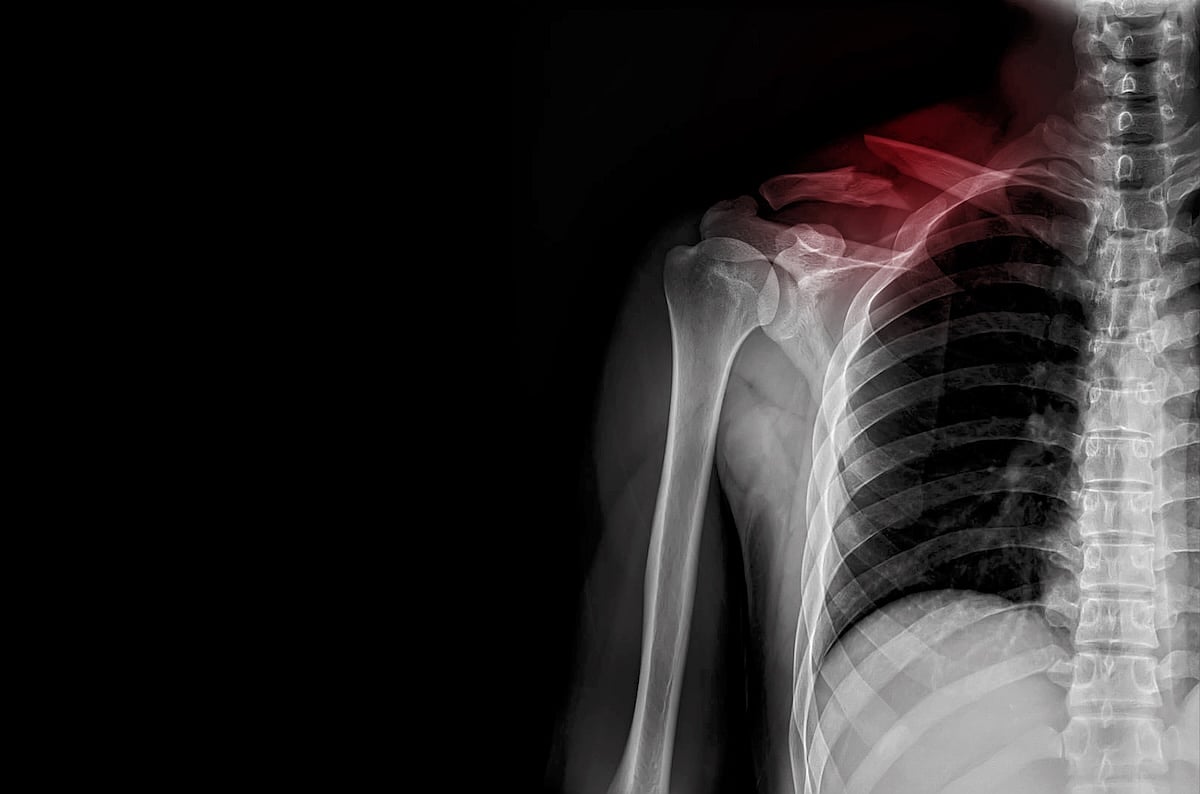
Broken Collarbone Hospitalizations Increase Among Children
More kids are being hospitalized for broken collarbones, a new study has found.
In fact, the hospitalization rate for broken collarbones more than doubled among children between 2014 and 2021, researchers reported.
This increase occurred even though the overall rate of childhood clavicle fractures remained relatively stable during th...
- Dennis Thompson HealthDay Reporter
- |
- July 9, 2025
- |
- Full Page
AI Displays Racial Bias Evaluating Mental Health Cases
AI programs can exhibit racial bias when evaluating patients for mental health problems, a new study says.
Psychiatric recommendations from four large language models (LLMs) changed when a patient’s record noted they were African American, researchers recently reported in the journal NPJ Digital Medicine.
“Most o...
- Dennis Thompson HealthDay Reporter
- |
- July 9, 2025
- |
- Full Page
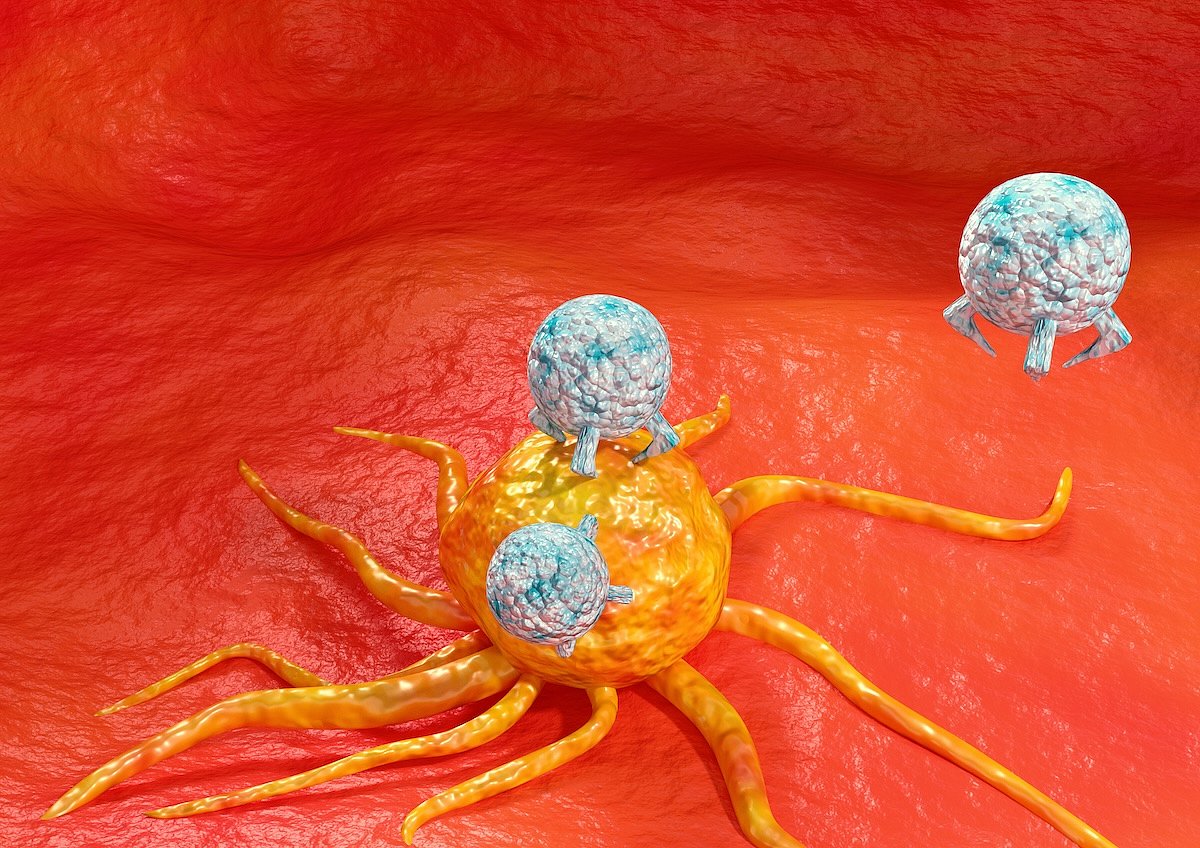
Insured? You're More Likely To Survive Cancer Through Immunotherapy Treatment
Powerful new immunotherapies are offering fresh hope for patients with many different types of cancer.
Unfortunately, that hope doesn’t extend to people without health insurance, a new study says.
Immune checkpoint inhibitors (ICIs) are revolutionizing cancer treatment by helping the immune system better find and attack cancer ...
- Dennis Thompson HealthDay Reporter
- |
- July 9, 2025
- |
- Full Page
Optimistic? Your Asthma Might Improve, Study Says
Want your asthma to improve? Cultivate a positive outlook, researchers say.
An asthma patient’s level of optimism or pessimism can influence how their symptoms progress, a new study says.
People who expect their asthma and health to get worse wind up reporting more symptoms over time, researchers reported recently in the journa...
- Dennis Thompson HealthDay Reporter
- |
- July 9, 2025
- |
- Full Page
These Items Sold at Costco Have Been Recalled — Check Your Home
If you shop at Costco, you may want to check your home for items that have recently been recalled.
In the past few months, the retailer has flagged nearly a dozen products due to safety or health risks.
Some were sold directly in Costco stores, while others were purchased through Costco Next, a program that lets shoppers buy items st...
- I. Edwards HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
U.S. Measles Cases Hit Highest Level Since Disease Was Eliminated in 2000
Measles cases in the United States have reached their highest level in 25 years, with more than 1,270 confirmed cases this year.
That number surpasses the last record of 1,274 cases set in 2019, according to new data from Johns Hopkins University.
Experts suspect the true number may be much higher, since many cases go unreported. So ...
- I. Edwards HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
Kids’ Health in U.S. Has Gotten Worse Over the Past 17 Years, Study Finds
The health of American kids has worsened over the past 17 years, with more now struggling with obesity, mental health problems and chronic illness, a new study shows.
Researchers used electronic health records, surveys and international data to look at nearly 170 health indicators. The takeaway: Across nearly every area studied, U.S. kids&...
- I. Edwards HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
Common Meds Aren't Linked To Inflammatory Bowel Disease, Study Says
There’s no evidence that common medications can trigger a chronic inflammatory bowel disease called microscopic colitis, a new study says.
Microscopic colitis is responsible for more than 30% of all chronic diarrhea cases in seniors, and cases are rising worldwide, researchers said in background notes.
Previous studies had sugg...
- Dennis Thompson HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
Three-Quarters of Stomach Cancers Could Be Prevented By Targeting One Type of Bacteria
Three-quarters of stomach cancer cases could be prevented if doctors eradicate infection by a common type of bacteria, a new study says.
The bacteria, Helicobacter pylori, is linked to 76% of future stomach cancer cases, researchers reported July 7 in the journal Nature Medicine.
Most stomach cancers “are...
- Dennis Thompson HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
Excess Weight Increases Risk of Health Double-Whammy Among Older Women
Older women carrying excess weight have a higher risk of a life-threatening double-whammy, a new study says.
Women past menopause with a higher body mass index (BMI) were more likely to develop breast cancer if they had heart disease, researchers reported July 7 in the journal Cancer. BMI is an estimate of body fat based on height...
- Dennis Thompson HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
Clash Of Drugs Impedes Lung Cancer Treatment, Lowers Survival
Two drugs used in lung cancer treatment appear to be tripping over each other, reducing patients’ chances for a cure, a new study says.
Corticosteroids are commonly prescribed to alleviate cancer-related symptoms in patients with non-small cell lung cancer, researchers said.
But these steroids appear to dampen the effectiveness...
- Dennis Thompson HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
More Florida Teens Strapping Up, Study Says
More Florida teens are roaming the streets packing heat, a new study says.
Handgun carrying among Florida middle and high school students increased by 65% between 2002 and 2022, researchers reported July 7 in the journal Pediatrics.
Teenage girls, middle school students and white children contributed substantially to this in...
- Dennis Thompson HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
A Single Disorder Upended Pennsylvania's Medical Marijuana Program
A single mood disorder might have driven a rapid increase in Pennsylvania’s medical marijuana program, a new study says.
Enrollment dramatically spiked after officials added anxiety to the list of conditions that could be treated with medical weed, researchers reported July 7 in the Annals of Internal Medicine.
Chronic...
- Dennis Thompson HealthDay Reporter
- |
- July 8, 2025
- |
- Full Page
U.S. Hospitals Face Shortages in Essential Staff Due to Foreign Residency Visa Delays
The Trump administration's recent travel and visa restrictions have left some hospitals in the United States without essential staff, according to a report from the Associated Press.
International doctors who were set to start their medical training this week are finding they are stumbling at the last hurdle -- a visa to enter the...
- Stephanie Brown HealthDay Reporter
- |
- July 7, 2025
- |
- Full Page
Six Key Traits That Make Someone 'Cool,' Study Finds
What does it take to be considered “cool”?
A new international study may have the answer — and it turns out cool people tend to act the same way no matter where they live.
Researchers from universities in Chile, the United States and beyond found that people seen as “cool” share six key personality...
- I. Edwards HealthDay Reporter
- |
- July 7, 2025
- |
- Full Page
Oregon Infants Sickened By Lead in Recalled Target Baby Food
MONDAY, July 7, 2025 — Two babies in Oregon got sick with lead poisoning after eating baby food from Target that was previously recalled, Oregon health officials said.
The food was part of the Good & Gather brand sold at Target stores and made by the company Fruselva. It was recalled back in March, but the Oregon Health Authority...
- I. Edwards HealthDay Reporter
- |
- July 7, 2025
- |
- Full Page
CDC Now Recommends RSV Vaccine for Some Adults 50+
Adults as young as 50 may now qualify for an RSV vaccine if they have certain health conditions, according to a quiet update from the U.S. Centers for Disease Control and Prevention (CDC).
This marks a change from the CDC’s previous recommendation, which only offered the shot to people 60 and older who were at high risk, The Asso...
- I. Edwards HealthDay Reporter
- |
- July 7, 2025
- |
- Full Page
Rheumatoid Arthritis Patients Benefit From Blood Flow-Restricted Strength Training
Folks who work out to ease their rheumatoid arthritis (RA) symptoms might find some relief from an unexpected source – a blood pressure cuff.
People who apply pneumatic cuffs to a limb while working out experience reduced pain and improved strength and physical performance, a small-scale study indicates.
This new form of exerci...
- Dennis Thompson HealthDay Reporter
- |
- July 7, 2025
- |
- Full Page
More Than 14 Million Will Die Following U.S. Foreign Aid Cuts
More than 14 million children and adults will die from preventable causes during the next five years as a result of U.S. foreign aid cuts, a new study projects.
Programs supported by the U.S. Agency for International Development (USAID) prevented 91 million deaths between 2001 and 2021 in low- and middle-income countries, researchers repor...
- Dennis Thompson HealthDay Reporter
- |
- July 7, 2025
- |
- Full Page